Views: 0 Author: Site Editor Publish Time: 2025-08-25 Origin: Site











Olympus EVIS X1 and FUJIFILM ELUXEO 8000 stand at the forefront of modern endoscopy, integrating cutting-edge imaging, artificial intelligence, and workflow enhancements. These medical endoscopes deliver superior visualization, supporting healthcare teams in both diagnostic and therapeutic procedures. Selecting between a Rigid Endoscope and a flexible endoscope matters, as each design influences procedural success. In clinical studies, advanced endoscope systems have improved medical care by reducing hospital stays and optimizing efficiency, benefiting both patients and healthcare providers.
Key features of the latest medical endoscopes:
High-definition imaging and color enhancement
AI-powered lesion detection
Streamlined workflow for healthcare teams
Rigid endoscopes offer superior image quality and stability, making them ideal for precise surgical procedures like laparoscopy and arthroscopy.
Flexible endoscopes provide excellent maneuverability to navigate curved and hard-to-reach body areas, improving patient comfort and access.
Advanced technologies such as AI, high-definition imaging, and robotic assistance enhance diagnostic accuracy and procedural safety in modern endoscopy.
Proper cleaning and sterilization are crucial, especially for flexible endoscopes, to reduce infection risks and ensure patient safety.
Choosing between rigid and flexible endoscopes depends on clinical needs, patient comfort, anatomical access, and procedure type to achieve the best outcomes.
Rigid endoscopes, also known as rigid tube endoscopes, feature a firm, inflexible metal tube that provides exceptional toughness and precision. This rigid skeleton allows surgeons to perform procedures with high stability. The design of a rigid-tube endoscope is straightforward, often resembling a straight or slightly curved rod with a fixed length and geometry. Unlike flexible endoscopes, rigid tube endoscopes do not bend or adapt to body curves. Instead, they offer a stable platform for direct visualization and precise manipulation.
Structural Comparison Table:
Structural Component | Rigid Endoscopes | Flexible Endoscopes |
|---|---|---|
Tube Material & Structure | Firm, inflexible metal tube (sheath) providing toughness and precision; acts as a rigid skeleton. | Coil of flexible tubing encapsulated in an elastic polyurethane outer jacket allowing bending and maneuverability. |
Design & Shape | Simple, straight or curved rod-like structure; fixed length and geometry. | Multiple parts including front tip, bending section, insertion tube, manipulation part, observation lens, image display. |
Viewing Capability | Fixed viewing angles (0°, 30°, 70°); provides a stable, direct, and clear view for precision tasks. | Bending section controlled by angulation wires allows up to 180° movement; adaptable to body curves and complex paths. |
Light Interface | Direct attachment to a light optical arm two-fiber interface for projecting light into compartments. | Integrated light guide bundles within the flexible tip for illumination. |
Functional Use | Preferred for surgeries requiring depth, stability, and precision (e.g., laparoscopy, arthroscopy). | Designed for navigation through natural body curves for diagnosis and treatment in complex anatomical areas. |
Rigid endoscopes deliver outstanding image quality due to their fixed optical pathways and stable design. The rigid structure ensures that the image remains clear and undistorted, which is essential for procedures requiring millimeter-scale precision. Surgeons rely on this clarity for tasks such as arthroscopy and laparoscopy, where spatial orientation and depth perception are critical. While flexible endoscopes have improved with advanced lens technology and digital imaging, rigid tube endoscopes still provide superior resolution and stability, especially in linear anatomical regions. This advantage makes them the preferred choice for many surgical applications where accuracy cannot be compromised.
Rigid endoscopes play a vital role in modern medical practice. They are widely used in orthopedic surgery, particularly for arthroscopy, where direct visualization of joints is necessary. Urology also benefits from rigid endoscopy, enabling minimally invasive procedures with reduced patient trauma. In gynecology, rigid tube endoscopes assist in laparoscopy to examine reproductive organs. Neurosurgeons use specialized rigid endoscopes for enhanced visualization of intracranial structures, improving safety and precision.
Common clinical applications include:
Arthroscopy for joint visualization and treatment
Laparoscopy for abdominal and pelvic procedures
Urological interventions
Microlaryngoscopy for vocal cord assessment
Neurosurgery for minimally invasive access to the brain
Advances such as single-use rigid endoscopes and smaller diameters have further reduced infection risks and improved patient recovery times. Enhanced imaging, including 4K UHD, continues to elevate the standard of care in these medical fields.

Flexible endoscopes feature a sophisticated design that allows them to bend and twist through complex anatomical pathways. The insertion tube of a flexible tube endoscope contains multiple layers, including a braided metal middle layer that provides both strength and flexibility. The articulating section uses interlocking rings or joints, which are controlled by wires. Physicians can manipulate control knobs on the handle to adjust the tension in these wires, allowing the distal tip to bend in multiple directions—sometimes up to 270 degrees. The outer casing, made from durable materials like polyurethane, protects the internal components while maintaining elasticity. These design elements enable flexible tube endoscopes to navigate tight spaces and natural body curves with high maneuverability. Newer flexible endoscope models may even include robotic or automated bending systems, further enhancing precision and reducing operator fatigue.
Tip: The combination of flexible materials and mechanical control systems in flexible tube endoscopes allows for smooth, controlled movement during medical procedures.
Flexible endoscopes excel in navigating intricate anatomical regions. Their flexibility allows them to move around curves and through narrow passages with minimal patient discomfort. The steerability of a flexible tube endoscope, provided by advanced control handles, lets practitioners precisely manipulate the tip’s angle and direction. Some systems offer 360-degree rotation and advanced control mechanisms, which enhance access to difficult-to-reach areas. Active and passive navigation techniques, such as magnetic actuation and robotic assistance, further improve tip stability and control. These features allow flexible endoscopy to reach and visualize anatomically challenging areas, improving both diagnostic and therapeutic outcomes.
Flexible endoscopes play a vital role in a wide range of medical procedures. Physicians use flexible tube endoscopes for nasal endoscopy, nasopharyngoscopy, and nasolaryngoscopy to diagnose and manage upper airway complaints. These procedures help identify conditions such as allergic rhinitis, laryngopharyngeal reflux, vocal cord polyps, and malignancies. In surgery, flexible endoscopes assist with preoperative diagnosis, intraoperative lesion localization, and postoperative follow-up. They also help manage complications like ulcers and retained stones. Flexible endoscopy is essential in procedures such as bronchoscopy, colonoscopy, and duodenoscopy. The modular design of flexible tube endoscopes allows adaptation for different anatomical regions, making them indispensable in both diagnostic and therapeutic interventions.
Understanding the structural differences between a rigid endoscope and a flexible endoscope is essential for healthcare professionals. These differences impact performance, image quality, and clinical applications. The table below summarizes the main distinctions:
Feature | Rigid Endoscopes | Flexible Endoscopes |
|---|---|---|
Tube Material | Metal tube providing strength, rigidity, and stability; acts as a solid skeleton for the device | Coil of flexible tubing encapsulated in an elastic polyurethane outer jacket, allowing bending and flexibility |
Flexibility | Inflexible, firm structure designed for precision and stability | Highly flexible with bending sections controlled by angulation wires enabling multi-directional movement |
Bending Mechanism | None; fixed geometry and length | Contains bending sections with connected metallic rings controlled by angulation wires for maneuverability |
Viewing Capabilities | Fixed viewing angles (0°, 30°, 70°), providing stable and continuous views for precise surgeries | Multi-directional viewing with ability to navigate through natural body curves, suitable for dynamic and hard-to-reach areas |
Structural Components | Simple rigid tube with integrated optical lenses and light channels | Complex assembly including front tip, bending section, insertion tube, manipulation part, observation lens, and display |
Outer Covering | Metal surface | Polyurethane outer jacket that maintains a complete seal and prevents fluid ingress |
Medical Application | Suited for surgeries requiring high precision and stability (e.g., laparoscopy, arthroscopy) | Ideal for diagnostic and therapeutic procedures requiring navigation through curved or narrow body passages |
Clinical research highlights that a rigid endoscope delivers higher spatial resolution and image stability due to its fixed structure. This allows advanced imaging methods, such as 4K UHD and fluorescence imaging, to achieve superior clarity. In contrast, a flexible endoscope offers greater maneuverability but faces challenges in maintaining image quality when bent. Advanced techniques help compensate for these limitations, but the rigid endoscope remains the standard for procedures demanding the highest image fidelity.
Note: Rigid endoscopes excel in image quality and stability, while flexible endoscopes provide unmatched access to complex anatomical regions.
Proper cleaning and sterilization of endoscopes are critical for patient safety and infection control in medical settings. Flexible endoscopes require thorough cleaning followed by sterilization. If sterilization is not possible, high-level disinfection (HLD) serves as the minimum standard. The ANSI/AAMI ST91 standard recommends sterilization for all flexible endoscopes, especially high-risk types like duodenoscopes and bronchoscopes, due to their complex design and increased infection risk.
Three validated sterilization methods for heat-sensitive flexible endoscopes include:
Ethylene Oxide (EtO) Sterilization
Vaporized Hydrogen Peroxide (VH2O2) Sterilization
Liquid Chemical Sterilization (LCS) using peracetic acid-based systems
Proper storage and transport of sterilized flexible endoscopes are essential to prevent contamination. Specialized drying and storage cabinets, along with secure transport systems, help maintain sterility. Recent studies show that improper cleaning of flexible endoscopes can lead to significant infection risks. For example, over 10,000 adverse event reports in the FDA MAUDE database from 2014 to 2021 describe contamination or infection risks linked to improper reprocessing. Duodenoscopes and bronchoscopes have been associated with outbreaks of multidrug-resistant organisms, with mortality rates reaching 50% or higher in some cases.
Endoscope Type | Infection Risk Evidence / Infection Rate Indicators |
|---|---|
Flexible Endoscopes (general) | Over 10,000 adverse event reports (2014-2021) in FDA MAUDE database describe contamination or infection risks linked to improper reprocessing. |
Duodenoscopes | Linked to multiple outbreaks of multidrug-resistant organisms (e.g., CRE) since 2014; FDA safety alerts issued; mortality rates up to 50% or higher; complex design impedes effective cleaning; some reduction in death reports by 2021 but risk remains significant. |
Gastroscopes | Largest increase in contamination reports (approx. 8,631% increase from 2014 to 2021); 3,797 relevant reports; no specific FDA safety communication yet; linked to multidrug-resistant infections with high mortality. |
Bronchoscopes | Reports increased nearly 400% from 52 (2014) to 259 (2021); linked to CRE infections; FDA issued two safety alerts (2015, 2021); mortality rates up to 50% or higher. |
Urological Endoscopes | Smallest increase in reports (17% increase recently); still linked to contamination risks and infections. |
ENT Endoscopes | Most marked increase recently (189% increase from 2020 to 2021), though absolute number of reports remains lowest (n=55 in 2021); linked to infections but simpler design. |
Colonoscopes | Lower reported infection risk compared to duodenoscopes; some cases linked to CRE infections; no recent FDA safety communication. |
Tip: Moving from high-level disinfection to sterilization for flexible endoscopes reduces infection risks, especially with multidrug-resistant organisms.
While the literature focuses on flexible endoscopes, rigid endoscopes generally have a simpler design, making them easier to clean and sterilize. This structural difference contributes to lower infection risks in rigid endoscopy.
Healthcare professionals must consider several clinical factors when choosing between a rigid endoscope and a flexible endoscope. The decision depends on image quality, stability, invasiveness, patient comfort, anatomical access, and procedure suitability.
Clinical Factor | Rigid Endoscope | Flexible Endoscope |
|---|---|---|
Image Quality | Higher resolution, advanced imaging systems | Lower image quality, less precise rendering |
Stability & Precision | Greater stability and precision during use | More delicate to handle, requires expertise |
Invasiveness | Requires larger incisions or openings | Less invasive, navigates curved anatomy easily |
Patient Comfort | Potentially more pain, longer recovery | More comfortable, less pain, shorter recovery |
Anatomical Access | Limited by rigid linear design | Can access hard-to-reach, curved anatomical areas |
Procedure Suitability | Neurosurgery, laparoscopic surgery, orthopedics | Pediatric cases, difficult-to-reach areas |
Risk Profile | Slightly higher risk of tissue damage | Lower risk of tissue damage |
Handling & Maintenance | Easier to handle, simpler maintenance | Requires specific training and rigorous cleaning |
Cost | Generally lower initial and maintenance costs | Higher initial and maintenance costs |
Clinical Context | Preferred when high precision and image quality needed | Preferred for patient comfort and complex anatomy |
For example, surgeons select a rigid endoscope for procedures that demand high-resolution imaging and precise instrument control, such as neurosurgery or laparoscopy. In contrast, a flexible endoscope is ideal for diagnostic procedures in the gastrointestinal tract, bronchoscopy, or pediatric cases, where patient comfort and access to curved anatomy are priorities.
Clinical Insight: The choice between rigid and flexible endoscopes directly affects medical outcomes, patient safety, and procedural efficiency. Healthcare teams must evaluate each case individually to ensure optimal results.
Recent advancements in medical technology have transformed the capabilities of the modern endoscope. Engineers have developed ultra-thin endoscopes, with diameters as small as 80 micrometers, allowing physicians to access delicate anatomical regions with minimal trauma. Confocal Laser Endomicroscopy (CLE) enables real-time cellular imaging during procedures, reducing the need for traditional biopsies. Capsule endoscopy introduces a swallowable camera that travels through the digestive tract, capturing images of areas that conventional scopes cannot reach. Wireless and remote-controlled instruments, such as the NaviCam capsule, offer greater comfort and flexibility for patients. Robotic endoscopy systems, including semi-autonomous robots, improve navigation and reduce operator fatigue. Enhanced therapeutic devices, such as advanced clipping and suturing tools, expand treatment options for gastrointestinal lesions.
The following list highlights significant technological advancements in endoscopy systems over the past five years:
Miniaturization of endoscopes for less invasive procedures
Confocal Laser Endomicroscopy for microscopic, real-time examination
Capsule endoscopy for hard-to-reach digestive tract areas
AI-powered lesion detection and diagnosis
Wireless and remote-controlled camera systems
Robotic navigation for increased efficiency
Advanced clipping and suturing devices for complex repairs
Technological Advancement | Description | Impact/Benefit | Examples |
|---|---|---|---|
High-Definition Imaging | Endoscopes with 650,000 pixels resolution enabling clearer images | Increased adenoma detection rate compared to conventional endoscopy | High-definition white light colonoscopy |
Devices Enhancing Mucosal Visualization | Tools that improve visualization of colonic folds and mucosa | Higher ADR by better viewing proximal colon areas | Cap-assisted colonoscopy, EndoRings, Endocuff |
Full-Spectrum Endoscopy Colonoscope | Colonoscope with 3 cameras providing 330-degree view | Higher ADR than standard forward-viewing colonoscopes | Full-spectrum colonoscope |
Retroflexion Techniques | Devices allowing retroflexion to view proximal and distal sides of folds | Increased ADR by visualizing hidden areas | RetroView, Third Eye Retroscope |
Endoscopic Clipping and Suturing Devices | Advanced clips and suturing systems for therapeutic interventions | Enables closure of perforations, bleeding control, and complex repairs | Through-the-scope clips, Over-the-scope clips (OTSC), OverStitch suturing system |
Imaging technology in medical endoscopy has advanced rapidly. High-definition and 4K ultra-HD imaging deliver higher image resolution, allowing clinicians to detect subtle abnormalities that might otherwise remain hidden. Flexible Spectral Imaging Color Enhancement (FICE) improves visualization of mucosal and vascular structures, leading to more accurate diagnoses of conditions such as Barrett’s esophagus and early gastric cancer. Optical Coherence Tomography (OCT) provides detailed imaging of tissue microstructure, supporting better lesion assessment. Narrow-Band Imaging (NBI) enhances visualization of blood vessels and mucosa, improving early cancer detection and lesion characterization.
Artificial intelligence now plays a central role in modern endoscopy systems. AI algorithms, including convolutional neural networks, process images in real time and provide rapid diagnostic feedback. These systems support both computer-aided detection (CADe) and computer-aided diagnosis (CADx), helping clinicians identify and characterize lesions with greater accuracy. AI-powered platforms, such as Medtronic’s GI Genius and Fujifilm’s CAD EYE, assist in real-time polyp detection and diagnosis. Capsule endoscopy benefits from AI by automating image analysis, reducing physician workload, and improving diagnostic sensitivity.
Key improvements in imaging and AI:
Real-time lesion detection and classification
Enhanced visualization of tissue architecture and vascular patterns
Automated image analysis for capsule endoscopy
Support for robotic navigation and scope management
Improved diagnostic accuracy and workflow efficiency
Robotic assistance has revolutionized therapeutic endoscopic procedures. Robotic wrists provide increased degrees of freedom, enabling precise internal movements and improved ergonomics. Systems like the MASTER and Endomaster EASE allow multitasking with various end effectors, facilitating optimal tissue traction and triangulation. Animal studies show that robotic suturing devices can close perforations and achieve hemostasis during endoscopic submucosal dissection (ESD), reducing the need for surgical intervention. In human case series, robotic systems have enabled complete gastric lesion resections without complications, demonstrating enhanced safety and precision.
Aspect | Robotic Endoscopy (Endomaster EASE System) | Conventional Endoscopy (Fujimoto et al.) | Conventional Endoscopy (Turiani Hourneaux de Moura et al.) |
|---|---|---|---|
Mean procedural time (gastric ESD) | 39 min (range 26–68 min) | 87.0 ± 43.1 min | N/A |
Lesion size (gastric) | 2.2 cm (range 1.5–3 cm) | 2.74 ± 1.00 cm | N/A |
Complete resection rate | 100% (5 patients, no complications) | N/A | N/A |
Perforation rate | 0% | 5.5% | 30% (robotic) vs 60% (conventional) |
Bleeding rate | 0% | 5.5% | N/A |
Mean procedural time (colonic ESD) | 34.1 min | 88.6 min | N/A |
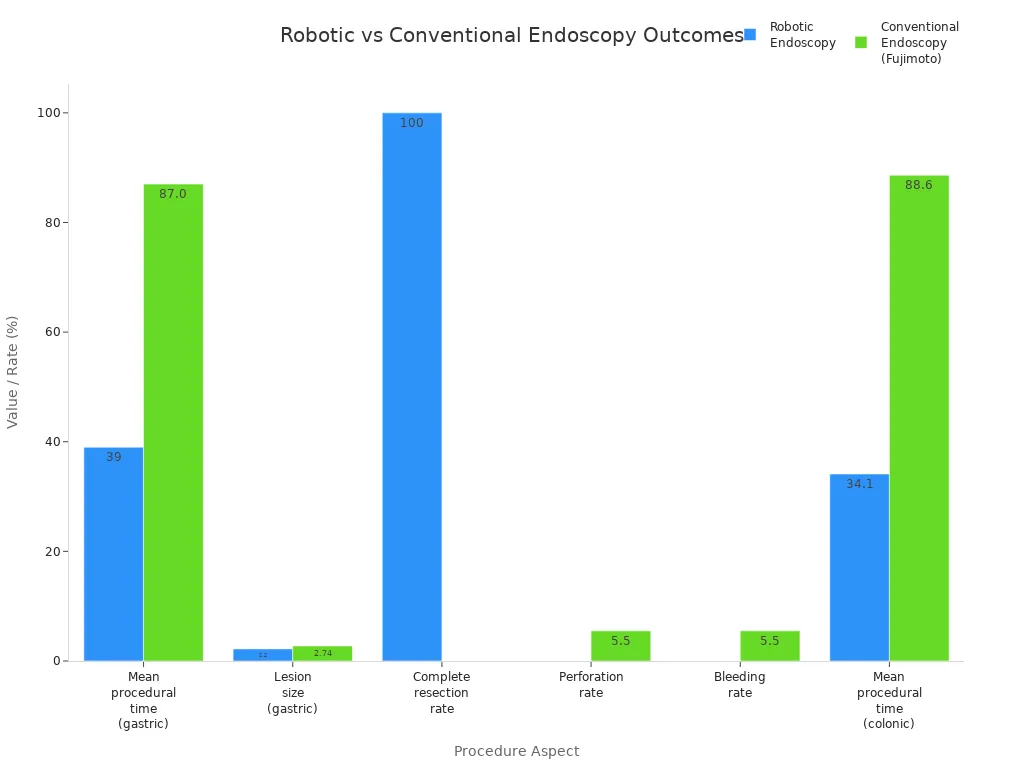
Robotic endoscopy systems mimic surgeon wrist articulation, enabling better tissue retraction and reducing complication rates in complex procedures. In animal trials, robotic needle holders and graspers applied surgical knots efficiently, demonstrating effective management of perforations. These innovations improve procedural safety, reduce operator fatigue, and enhance patient outcomes in advanced medical practice.
Advanced endoscopy systems have transformed surgical procedures across multiple medical specialties. Surgeons now perform a wide range of minimally invasive surgical procedures using both rigid and flexible endoscopes. Rigid endoscopes remain essential in surgical operations such as laparoscopy, arthroscopy, and the removal of esophageal foreign bodies. Flexible endoscopes, on the other hand, enable complex interventions in the gastrointestinal tract and respiratory system. The table below highlights common surgical procedures and their medical specialty focus:
Procedure Name | Surgical Application / Medical Specialty Focus |
|---|---|
Barrx™ Radiofrequency Ablation | Treatment of Barrett's esophagus to remove precancerous cells in the upper GI tract, preventing esophageal cancer. |
Endoluminal Stenting | Management of obstructions in esophagus, small bowel, or colon due to cancerous or non-cancerous blockages. |
Endoscopic Retrograde Cholangiopancreatography (ERCP) | Removal of gallstones, treatment of obstructive jaundice, pancreatic cancer, biliary strictures, and pancreatic cysts. |
Endoscopic Mucosal Resection (EMR) | Removal of early-stage cancers, precancerous growths, tumors, and large polyps in the digestive tract without open surgery. |
Endoscopic Suturing | Minimally invasive closure of defects, securing stents, managing fistulas, and revising bariatric surgeries. |
Peroral Endoscopic Myotomy (POEM) | Treatment of achalasia and spastic esophageal disorders by cutting muscle fibers of the lower esophageal sphincter. |
Endoscopic Submucosal Dissection (ESD) | Removal of deep tumors and polyps with precise dissection to avoid damage to surrounding tissue, alternative to open surgery. |
Endoscopic Wound Vacuum Placement | Healing of difficult wounds, leaks, or perforations in the esophagus, stomach, or intestines using vacuum-assisted closure. |
Healthcare teams select the appropriate endoscope based on the medical procedure, anatomical location, and patient needs.
Modern endoscopic procedures have improved medical diagnostics by providing enhanced visualization and accuracy. Chromoendoscopy, narrow-band imaging, and probe-based confocal laser endomicroscopy allow clinicians to detect disease at earlier stages. Artificial intelligence integrated into endoscopy systems assists in identifying abnormalities, improving diagnostic accuracy. Robotic-assisted endoscopy offers greater precision, especially in tight anatomical spaces. Fluoroscopy combined with endoscopy provides real-time guidance, increasing safety during complex diagnostic procedures. These advancements reduce the need for open surgery and expand treatment options for patients.
Advanced endoscopy systems have led to better patient outcomes in healthcare. Quality improvement programs have increased Adenoma Detection Rate (ADR) from 10.8% to 20%, with improvements in polyp detection and procedural success rates. The chart below shows key statistics for common endoscopic procedures:
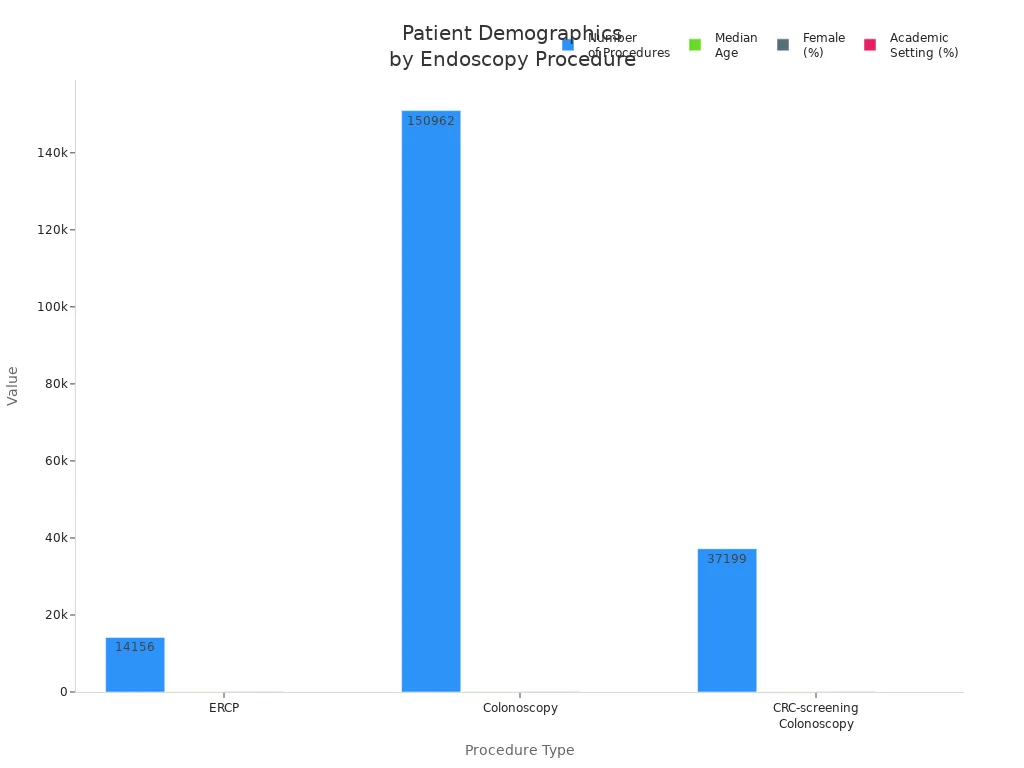
Flexible endoscopes, used through natural body openings, minimize trauma and allow most patients to resume normal activities within 24 hours to a few days. Rigid endoscopes, while effective for certain surgical procedures, often require incisions and longer recovery times. Continuous monitoring of complications and detection rates supports ongoing improvements in patient safety and the effectiveness of endoscopic examination in medical care.
Healthcare professionals must evaluate several factors when selecting an endoscopy system for their facility. They look for customization options in reporting, allowing physicians to capture all relevant details. Integration of multimedia elements, such as images and videos, enhances documentation. Centralized data aggregation reduces manual errors and streamlines workflow. Security and regulatory compliance, including encryption and adherence to HIPAA and GDPR, remain essential. Facilities benefit from scalable and modular designs that can grow with practice needs. Comprehensive training and responsive support ensure smooth implementation. Transparent pricing models help administrators assess long-term savings and return on investment. Advanced systems offer embedded analytics for clinical and operational insights. Compatibility with existing hospital networks and EMR/EHR systems supports seamless integration. High-resolution imaging and user-friendly interfaces improve diagnostic quality and efficiency. Efficient data management, including intelligent categorization and secure archival, further supports clinical operations.
Tip: Vendor-neutral integration allows facilities to use diverse endoscopy camera systems and medical record databases, supporting adaptability from single suites to large enterprises.
Clinicians must consider patient-centered factors when choosing between rigid and flexible endoscopes. The table below outlines key differences:
Patient Factor | Flexible Endoscopy Characteristics | Rigid Endoscopy Characteristics |
|---|---|---|
Age | Preferred for most; sedation/local anesthesia | Preferred in children needing airway protection |
Clinical Condition | Suitable for stable patients; less invasive | Best for sharp-pointed foreign bodies, upper esophagus |
Patient Compliance | Better comfort and tolerance | Used when compliance is low, under general anesthesia |
Anesthesia Risk (ASA Score) | Feasible with lower risk | Recommended when general anesthesia is needed |
Respiratory Symptoms | Preferred if no airway compromise | Best if airway protection is required |
Type of Foreign Body | Effective for blunt objects | Advantageous for sharp or large objects in upper esophagus |
Anatomical Site | Effective except upper esophagus | Better exposure for upper esophageal cases |
Patient Comfort and Safety | Higher comfort, lower complication rate | Requires general anesthesia, offers airway protection |
Cost and Hospitalization | Cost-effective, often outpatient | Usually requires hospitalization |
Physician Expertise | Widely available | Requires ENT specialist |
Patient safety remains the top priority. Flexible endoscopy often provides greater comfort and lower complication rates, while rigid endoscopy offers advantages in specific clinical scenarios.
The future of endoscopy systems will bring rapid innovation. Subspecialization within endoscopy is increasing, with practitioners focusing on specific anatomical areas. Miniaturization enables new diagnostic and therapeutic procedures, such as advanced cholangioscopy. Wireless capsule and balloon-assisted technologies expand access to difficult regions. Improvements in optics and high-definition imaging enhance early detection and clinical outcomes. Selective optical imaging techniques may reduce the need for invasive biopsies.
AI-enabled cloud endoscopy will transform surgical visualization and navigation.
Controllable capsule endoscopy and single-use endoscopes with enhanced steering will improve precision and patient safety.
4K UHD displays and AI-powered detection systems will support better lesion identification.
Virtual reality and simulation training will help surgeons master new technologies.
IoT connectivity will optimize workflows by integrating with hospital information systems.
Regulatory frameworks and government incentives will promote adoption of advanced imaging.
Sustainability and digital transformation will shape product development and healthcare practices.
Healthcare providers must stay informed about these trends to ensure the best outcomes for patients and maintain high standards of safety.
Olympus EVIS X1 stands as the most advanced endoscopy system, offering innovations like EDOF™ and TXI™ that deliver sharper images and higher adenoma detection rates. Clinicians improve patient outcomes and procedural efficiency by selecting the right endoscope—rigid endoscope or flexible—based on anatomy and procedure. New technologies, including steerable capsules and robotic platforms, continue to expand diagnostic and therapeutic options. Staying informed about these advancements ensures the best care for every patient.
A rigid endoscope uses a firm metal tube to provide stable, high-resolution images during surgical procedures. Surgeons prefer rigid endoscopes for tasks that require precise visualization and control, such as laparoscopy and arthroscopy.
A rigid endoscope features a straight, inflexible design. Flexible endoscopes bend and navigate curved anatomy. Rigid endoscopes deliver sharper images and greater stability, while flexible models offer better access to complex regions.
Clinicians select a semi rigid endoscope for procedures that need both stability and some flexibility. Semi rigid endoscopes work well in areas where a rigid endoscope cannot reach but where full flexibility is not required.
Rigid endoscopes have a simple structure, making cleaning and sterilization easier. Healthcare teams use standard sterilization methods to reduce infection risks. Proper maintenance ensures safe and effective use of rigid endoscopes.
Rigid endoscopes are suitable for pediatric cases that require airway protection or removal of sharp foreign bodies. Physicians choose rigid endoscopes for children when safety and precise control are essential.
