Views: 0 Author: Site Editor Publish Time: 2025-09-22 Origin: Site











You can keep endoscope lenses clean and clear by following strict cleaning routines and careful handling. Clean lenses give you sharp images, which is vital for accurate procedures. Clinical studies show that regular cleaning improves optical clarity in the endoscope, ensuring you always see details clearly. Although better cleaning does not directly lower complication rates, it helps you avoid cloudiness and maintain reliable performance. Simple habits like gentle wiping and proper storage prevent scratches and damage.
Regularly clean endoscope lenses after each use to maintain sharp image quality and prevent contamination.
Use approved cleaning agents and gentle techniques to avoid scratches and damage to the lens surface.
Properly store endoscopes in designated cabinets to protect them from dust and physical harm.
Conduct routine inspections to catch wear or contamination early, ensuring reliable performance.
Follow a structured daily maintenance checklist to extend the lifespan of your endoscope and enhance patient safety.
You rely on clear, sharp images from your endoscope to make accurate clinical decisions. The objective lens at the tip of the endoscope captures every detail inside the body. If you allow dust, debris, or scratches to accumulate, the lens will blur images and obscure critical features. Regular cleaning and inspection of endoscope lenses help you maintain high image quality.
A dirty lens can cause cloudiness and reduce resolution.
Scratches or residue may hide small lesions or abnormalities.
Consistent cleaning ensures you see the true condition of tissues.
You must protect your patients from infection control risks during every procedure. Contaminated endoscopes can introduce harmful microorganisms into the gastrointestinal tract, leading to severe infections.
Contamination of endoscopes with waterborne, gram-negative bacteria has been linked to adverse patient outcomes. Unless the rinse water is monitored to evaluate its microbial quality and content, the potential exists for the rinse water to contain pathogenic microorganisms capable of re-contaminating the endoscope during terminal water rinsing, compromising the effectiveness of the reprocessing procedure, invalidating the disinfection claim, and posing a risk of nosocomial infection.
A study from Johns Hopkins revealed that infection rates after upper endoscopies and colonoscopies were much higher than previously estimated. You must pay close attention to cleaning and drying steps to prevent transmission of bacteria such as Pseudomonas aeruginosa.
Failure to dry the endoscope can render the reprocessing procedure invalid and clinical use of the endoscope an infection risk. The contribution of post-processing in general and drying in particular to the prevention of disease transmission via a GI endoscope cannot be overstated.
You can avoid costly repairs and downtime by using proper cleaning techniques. Physical damage often occurs when you use abrasive materials or excessive force. Chemical damage may result from using inappropriate cleaning agents.
Mechanical interactions, such as rough wiping, can scratch the lens surface.
Strong chemicals may erode or cloud the lens.
Ultrasonic agitation can cause vibrations that damage sensitive components.
If you follow manufacturer guidelines and use gentle cleaning methods, you extend the lifespan of your endoscope lenses and maintain optimal performance.
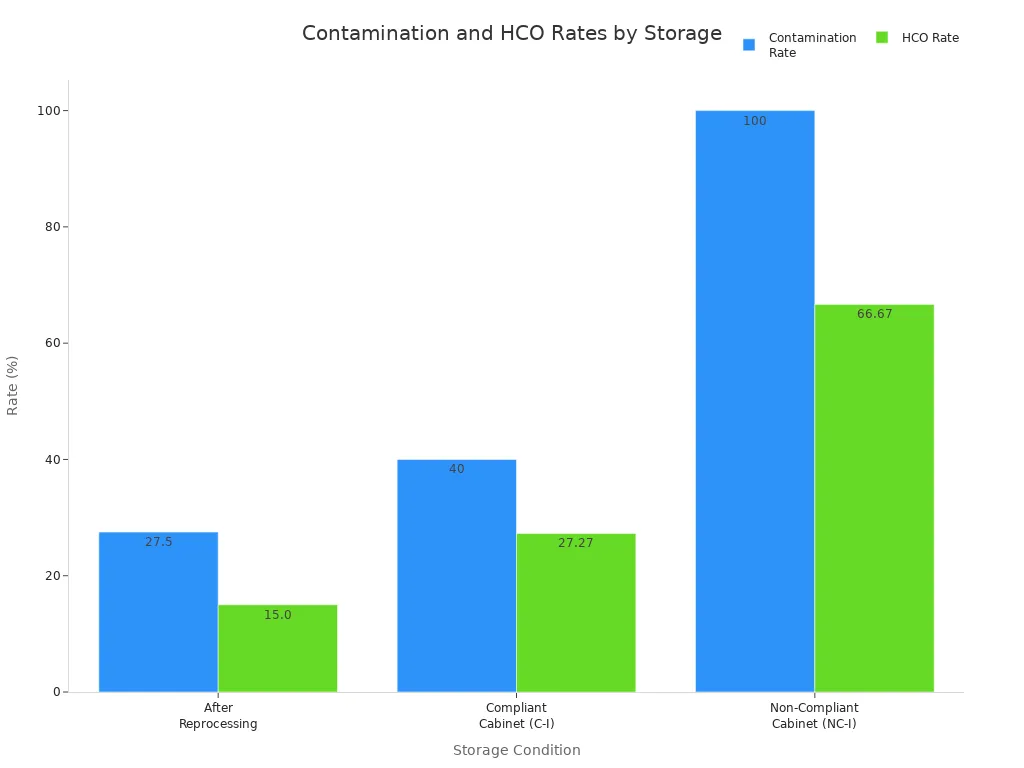
Storage Condition | Contamination Rate | HCO Rate |
|---|---|---|
After Reprocessing | 27.5% | 15.00% |
Compliant Cabinet (C-I) | 40% | 27.27% |
Non-Compliant Cabinet(NC-I) | 100% | 66.67% |
More health care-associated infections are related to contaminated endoscopes than to any other medical device. Despite strict guidelines, contamination and transmission of microorganisms continue to occur.
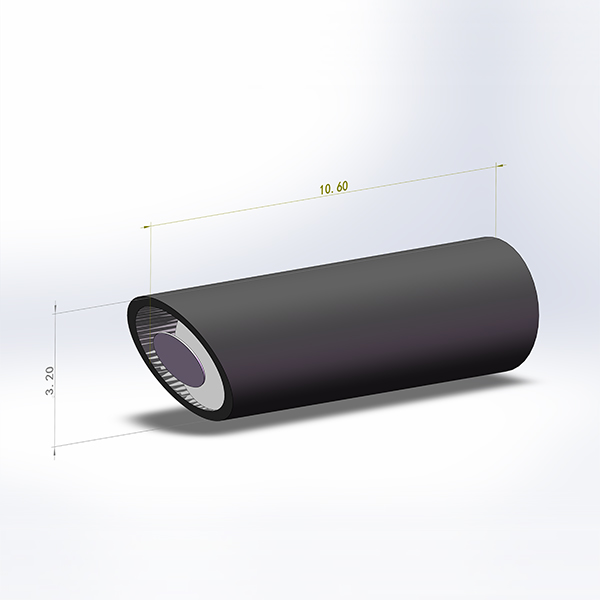
You need the right materials to clean your endoscope lenses safely and effectively. Using approved agents and tools helps you avoid scratches, cloudiness, and damage to high precision optical glass endoscope lens for medical use. The following table lists recommended cleaning agents and their purposes:
Cleaning Agent Type | Purpose |
|---|---|
Enzymatic Cleaners | Break down organic materials like proteins, fats, and carbohydrates for effective cleaning. |
Neutral Detergents | Non-corrosive agents safe for delicate materials, effective when combined with surfactants. |
Surfactants | Enhance cleaning action by reducing surface tension, allowing better penetration and removal of soils. |
You should also prepare lint-free cloths, disposable brushes, gauze sponges, and compressed air. These tools help you remove debris and dust from the lens surface without causing scratches.
Tip: Always use manufacturer-recommended cleaning agents and accessories to protect your gastrointestinal endoscope and maintain lens clarity.
Proper preparation ensures optimal cleaning results and protects your endoscope lenses from damage. Follow these steps before you begin:
Start pre-cleaning immediately after use by removing disposable elements and flushing channels with an enzymatic or detergent-based solution.
Conduct a comprehensive leak test to confirm the integrity of your endoscope.
Wear personal protective equipment and use specially designed brushes to clean both external surfaces and internal channels.
Rinse with sterile water and dry completely to prevent microbial growth.
Immerse the endoscope in a high-level disinfectant solution, following the manufacturer's recommended contact time.
You should never skip these steps, as they help prevent biofilm formation and ensure the lens remains clear for future procedures.
You must follow a systematic approach to cleaning your endoscope lenses. This process protects the high precision optical glass endoscope lens for medical applications and ensures reliable performance.
Pre-clean your scope immediately after use to prevent biofilm buildup. Wipe the insertion tube and soak detachable components in detergent solution.
Perform a leak test to check for damage and ensure proper disinfection.
Manually brush and flush all components. Immerse the scope in cleaner and scrub channels and ports thoroughly.
Rinse with clean water, wipe down, and dry the inside with forced air.
Disinfect according to manufacturer instructions. Soak the scope and remove disinfectant thoroughly.
Flush with 70% alcohol to promote drying and prevent bacterial growth, then dry with forced air.
Store the scope vertically and document the process for quality assurance.
Note: Avoid touching the eyepiece or objective lens directly. Use gauze sponges and enzymatic cleaning solution for debris. Always clean with a lint-free cloth and manufacturer-recommended detergent.
Manual wiping and lens irrigation systems both play important roles in maintaining lens clarity. Start with compressed air or a lens-cleaning brush to remove dust. Pay close attention to cleaning channels, as neglecting them can lead to contamination and cloudiness.
Drying is a critical step in the cleaning process. Incomplete drying can leave residue and cause cloudiness on your endoscope lenses. You should use automated drying processes or drying cabinets that circulate filtered air to completely dry surfaces and channels. The drying duration varies from 90 minutes to several hours, depending on the type of gastrointestinal endoscope.
Forced-air drying systems push filtered air through the channels to remove moisture.
These systems work well before placing scopes in conventional storage cabinets.
Tip: Always ensure all cleaning solution is dried to prevent cloudiness and maintain the performance of your high precision optical glass endoscope lens for medical use.
Common mistakes include failing to dry the scope completely, mishandling during transport, and neglecting to replace fragile accessories. You can avoid these issues by following a strict drying protocol and inspecting your endoscope after each cleaning cycle.
You must handle your endoscope with care to preserve lens clarity and extend device life. Avoid tightly coiling the insertion tube, as this can cause kinks and stress on the lens. Always support the scope during movement and cleaning.
Regular cleaning of the objective lens prevents scratches and dirt buildup, which can blur images.
Careful handling reduces the risk of accidental drops or impacts.
Store the distal end separately from the control body and connector to prevent contact damage.
Tip: Gentle handling is a key part of effective endoscope care and helps maintain high precision optical glass endoscope lens for medical use.
Proper endoscope storage protects your device from contamination and physical damage.
Store endoscopes in cabinets designed specifically for endoscope storage to shield them from dust and accidental knocks.
Hang scopes vertically to facilitate drying and prevent contamination.
Ensure the light guide and insertion tubes hang freely, avoiding tangling with other equipment.
Use tip protectors during storage to safeguard the delicate distal end.
Keep scopes in a dry environment, within the ideal temperature range, and inside a packaging box when not in use.
Note: Disinfected scopes should hang vertically in a dedicated cabinet, with the distal end off the floor. Forced medical grade air drying before storage reduces microbiological growth.
Safe transport is essential for protecting the lens and distal tip. You should use tip protectors and padded containers designed for medical scopes. Improper transportation can lead to broken lenses or kinks in the insertion tube, increasing the risk of device malfunction and infection. Solutions like ETS Plus and PROTECH provide secure options for moving scopes between locations, enhancing patient safety and minimizing damage.
Routine inspection helps you detect wear or contamination early.
Evidence Description | Frequency Recommendation |
|---|---|
Return duodenoscopes to the manufacturer for inspection and maintenance | Every six months |
Perform detailed visual inspection of the endoscope | More frequently than annually |
Regular inspections and maintenance checks by certified professionals reduce repair frequency and help maintain optimal image quality. Over three years, routine inspections resulted in a low number of repairs due to early defect detection.
Callout: Neglecting preventive care can lead to image degradation, increased risk of cross-infection, and costly device damage. Consistent endoscope care ensures your gastrointestinal endoscope remains reliable for every procedure.
You may encounter fogging on endoscope lenses during procedures. Fogging can obscure your view and compromise patient safety. Preheating the endoscope to around 50 °C helps reduce fogging, but the effect may fade as the device cools. Surfactant solutions, such as FRED and Ultra-Stop, modify surface tension and limit droplet formation. Gas insufflation, especially with carbon dioxide, clears fogging without removing the endoscope. These methods help you maintain lens clarity and minimize interruptions.
Tip: Always check the temperature and use approved surfactant solutions before starting a procedure to prevent fogging.
Scratches on endoscope lenses can degrade image quality and lead to costly repair. You can avoid scratches by following these steps:
Prevent impact damage by handling the distal end carefully during transport and maintenance.
Use only manufacturer-approved cleaning tools to avoid abrasive contact.
Keep the lens dry to prevent fluid invasion and internal damage.
Inspect your endoscope regularly to catch early signs of wear.
Store the device in a ventilated cabinet with the distal end hanging freely.
Routine inspection and proper storage protect your investment and reduce the need for frequent repair.
Stains can form on endoscope lenses after exposure to organic material. You should use enzymatic cleaning agents to break down proteins and fats. Non-linting wipes, sponges, or soft cloths clean the exterior without scratching. Specialized brushes, especially channel brushes, reach difficult areas and remove stubborn stains. Consistent cleaning with these tools keeps your lens clear and ready for use.
Cloudiness often develops during long procedures, especially when protein or oil adheres to the lens. Intraoperative bleeding and submucosal fat deposition in the stomach increase the risk of cloudiness. Cleastay, a novel lens cleaner, has shown significant results in reducing cloudiness. You should clean the lens promptly and use recommended cleaning agents to restore clarity.
You must seek professional repair when you notice tears in the bending rubber, kinks in cables, or fluid invasion. Minor repairs usually cost between $45 and $500. Major repairs range from $700 to $4,500. Complete refurbishments may cost up to $4,500. Timely repair prevents further damage and ensures your endoscope remains safe and effective for clinical use.
Alert: Ignoring signs of damage can lead to expensive repair and compromise patient safety. Schedule professional repair as soon as you detect any malfunction.
Maintaining your endoscope requires a consistent daily routine. You protect image quality and patient safety by following a structured checklist. This approach helps you prevent contamination and extend the lifespan of your equipment.
You should perform quick cleaning immediately after each use. Follow these steps to keep your endoscope ready for the next procedure:
Place the scope in a container with enzymatic cleaner to prevent soil from drying.
Inject the cleaning solution into all lumens for thorough contact.
Clean the telescope lenses and light post gently with a manufacturer-recommended detergent and a soft, lint-free cloth.
Rinse under running water. Use isopropyl alcohol on cotton if recommended to remove residue.
Inspect the image and light clarity before storage.
Tip: Always avoid touching the eyepiece or objective lens directly. Use Optic Preps and Chemswab alcohol swabs for lens cleaning.
You need to inspect your endoscope daily to ensure optimal performance. Include these steps in your routine:
Clean lenses to remove blood, tissue, and debris.
Check for any signs of damage or wear.
Replace worn or damaged lenses promptly to maintain image quality.
Test the light source by turning it on and checking intensity.
Perform a white balance test for the clearest display.
Callout: Regular inspection helps you catch problems early and maintain reliable performance.
Proper storage keeps your endoscope free from contamination and damage. Follow these guidelines:
Dry endoscope channels with forced air flow for at least 10 minutes.
Store scopes in drying cabinets that circulate filtered air.
Avoid using syringes for channel drying.
Use cabinets that can be disinfected and store scopes vertically.
Conduct risk assessments for safe storage duration.
Aspect | Description |
|---|---|
Designated Areas | Separate spaces for disinfection and manual cleaning improve safety. |
Visual Inspection | Always inspect for cleanliness before high-level disinfection. |
Quality Assurance | Monitor all aspects of endoscope processing daily. |
Note: Storing your endoscope in a closed, clean cabinet reduces microbial growth and preserves lens clarity.
You protect endoscope lenses by following daily cleaning, careful handling, and proper storage. Regular maintenance keeps your endoscope performing at its best and extends its lifespan.
Cleaning and sterilizing equipment reduces dust and debris that can damage delicate parts.
Studies show that proper reprocessing allows safe storage for up to 21 days with minimal risk.
Healthcare facilities track improvements by assessing equipment condition, procedure quality, and safety outcomes.
Consistent care ensures clear images and reliable performance for every procedure.
You should clean Endoscope Lenses after every procedure. This habit keeps your High Precision Optical Glass Endoscope Lens for Medical clear and safe. Regular cleaning prevents cloudiness and contamination in your gastrointestinal endoscope.
Use enzymatic cleaners and neutral detergents approved for High Precision Optical Glass Endoscope Lens for Medical. These agents remove debris from your gastrointestinal endoscope without damaging the lens surface.
You can use alcohol wipes designed for medical optics. Always check manufacturer guidelines for your High Precision Optical Glass Endoscope Lens for Medical. Alcohol wipes help remove stains and keep your gastrointestinal endoscope lens clear.
Handle your Endoscope Lenses gently. Use only lint-free cloths and approved brushes for High Precision Optical Glass Endoscope Lens for Medical. Store your gastrointestinal endoscope in a protective cabinet with tip protectors.
Clean your Endoscope Lenses immediately with recommended solutions. If cloudiness persists, inspect your High Precision Optical Glass Endoscope Lens for Medical for damage. Seek professional repair for your gastrointestinal endoscope if clarity does not return.
